Advocacy in Action - Merit-based Incentive Payment System (MIPS) Deadline
Carter J. Alleman, J.D.
Reporting One Measure Saves You Money – MIPS DEADLINE MARCH 31
Deadlines are fast approaching to submit data for the 2017 Merit-based Incentive Payment System (MIPS) performance period. Key dates are as follows:
•
March 1 to submit 2017 data for the Quality performance category via claims
•
March 16 at 8:00 pm Eastern time for group reporting via the Centers for Medicare and Medicaid Services (CMS) web interface
•
March 31 for all other MIPS reporting, including the MIPS data submission feature
Note that you can update your data up to the March 31 deadline. The data submission feature doesn’t have a “save” or “submit” button. Instead, it automatically updates as you enter data. You’ll see your initial scores by performance category, indicating that CMS has received your data. If your file fails to upload, you’ll get a message noting that problem.
Users can submit data as often as they like. The data submission feature will help you identify any underperforming measures and any issues with your data. Starting your data entry early gives you time to resolve performance and data issues before the March 31 deadline.
The Quality Payment Program(QPP) became live on January 1, 2017. This year serves as a transition year for doctors to participate in the QPP, during which the only physicians who will experience a -4 percent payment penalty in 2019 are those who choose not to report any performance data. Physicians can avoid the payment penalty in 2019 by reporting for one patient on one quality measure, one improvement activity, or the 4 required Advancing Care Information (ACI) measures in 2017. Physicians who wish to possibly qualify for a positive payment adjustment must report more than the minimum one patient for one quality measure, improvement activity or the 4 required ACI measures.
CMS even created a pick your own pace program to encourage data submission whereby any data submission may result in a positive net payment adjustment.
First Option: Test the Quality Payment Program
With this option, as long as you submit some data to the Quality Payment Program, including data from after January 1, 2017, you will avoid a negative payment adjustment. This first option is designed to ensure that your system is working and that you are prepared for broader participation in 2018 and 2019 as you learn more.
Second Option: Participate for part of the calendar year
You may choose to submit Quality Payment Program information for a reduced number of days. This means your first performance period could begin later than January 1, 2017 and your practice could still qualify for a small positive payment adjustment. For example, if you submit information for part of the calendar year for quality measures, how your practice uses technology, and what improvement activities your practice is undertaking, you could qualify for a small positive payment adjustment. You could select from the list of quality measures and improvement activities available under the Quality Payment Program.
If you do NOT submit any data, you will receive an automatic negative 4% payment adjustment for the 2019 payment cycle.
How to participate and avoid the 4% reduction:
The American College of Osteopathic Surgeons do not support nor endorse any measure listed below. The measure is selected as an example for educational purposes only.
1.
Go to
https://qpp.cms.gov/
2.
Enter your
National Provider Identifier (NPI) number.
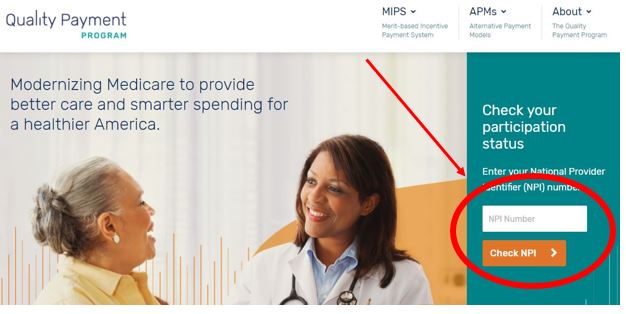
This will tell you whether you are eligible to participate in the MIPS program and whether you qualify for an exemption from participation. If you qualify for an exemption stop here. If not, continue.
3.
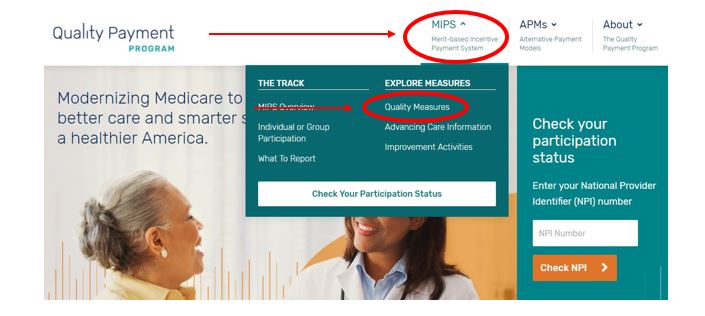
Click on
Explore Measure located on the top of the screen. Select
Quality Measures from drop down menu
4.
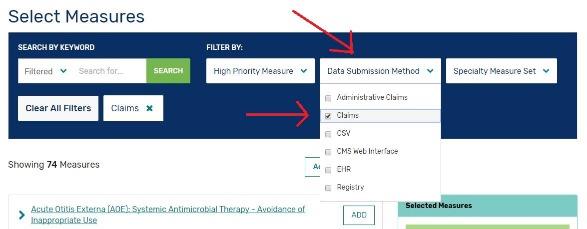
Scroll down to the middle of the page to see available measures. Click on
Data Submission Method and select
CLAIM, to the right select your specialty measure set (if available)
5.
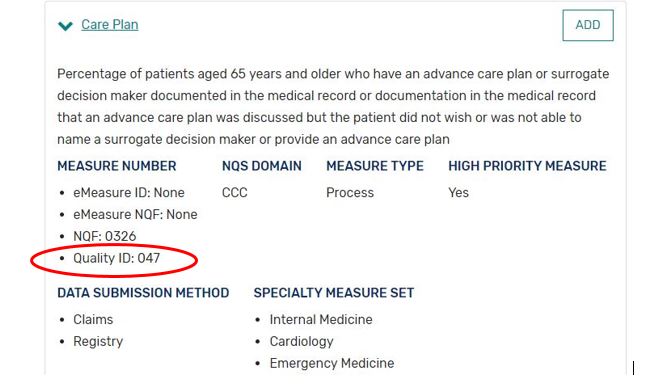
Select a measure and locate the
Quality ID number
6.
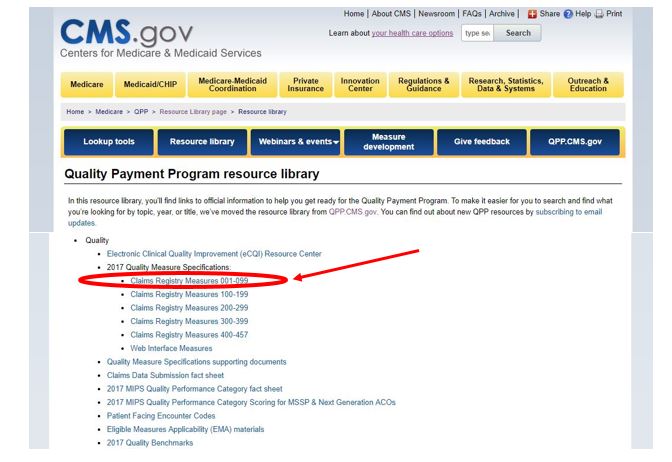
Go to
Quality Payment Program resource library and scroll to the middle of the page. Here you will find the
2017 Quality Measure Specifications. Match your selected
Quality ID number with the
Claims Registry Measure sets. Download and unzip the file.
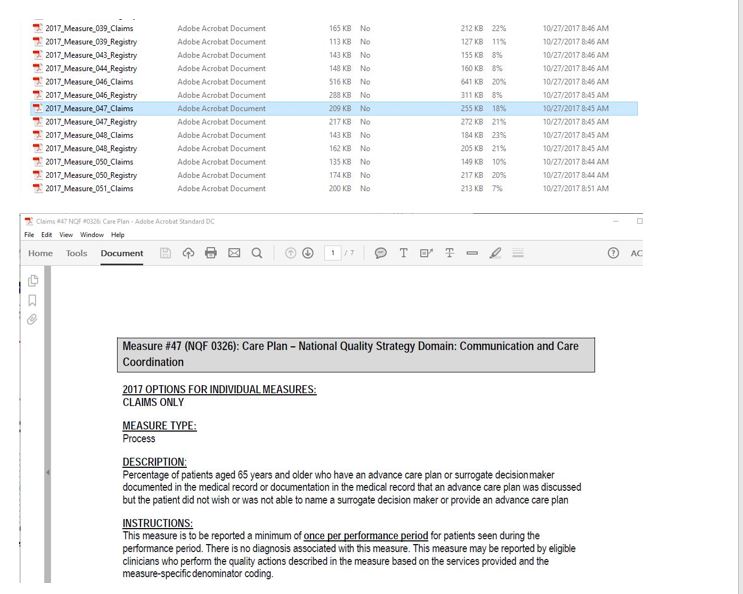
7.
After the file is unzipped, locate your measure using the
Quality ID number and open the corresponding file named
Claims. This will give you the instructions on how to complete this measure.
8.
Fill out your
1500 billing form and submit to your Medicare Administrative Contractor.
For further information regarding filling out the 1500 form please see the guide from the American Medical Association by
clicking here .
Additional Resources:
Clinicians in small practices, including those in rural locations, health professional shortage areas, and medically underserved areas are a vital part of our healthcare system. You provide critical services and access to health care for many Medicare patients. Check out
the flexible options that CMS provides to help you actively participate in the Quality Payment Program.