Advocacy Corner
Carter L. Alleman, J.D.
Stopping Surprise Billing Legislation
Reacting to the increase in reported surprise billing incidents in the media, Congress is releasing legislation to stop the practice. There are three instances where this occurs: emergency care, in-network facility with out-of-network providers, and in-network provider at an out-of-network facility. In all these instances the goal is to remove the patient from the billing dispute between the insurance company and the provider. It is at that point where the hair splitting begins in the proposed legislation as to who gets paid, how can disputes be settled, and what modes and methods are allowed.
The following is a brief outline of each of the proposed legislation currently being discussed. At the end of the legislation is a brief primer on the payment methods.
No Surprises Act
House Energy and Commerce Committee leadership released a bipartisan draft bill to address the issue of surprise insurance gaps during a stakeholder meeting, making it the first piece of surprise billing legislation from a committee with health care jurisdiction this year. The proposal, unveiled by Chairman Frank Pallone (D-N.J.) and Ranking Member Greg Walden (R-Ore.), is in line with the call for action and principles previously outlined by the White House. It would require hospitals and physicians to notify patients both in writing and orally when they are going to be treated by an out-of- network provider. The bill would prohibit surprise charges for emergency care and require insurers to treat out-of-network emergency care as in-network for the purpose of enrollee cost-sharing and out-of-pocket obligations.
The No Surprises Act draft would rely upon negotiated in-network rates to resolve out-of-network payment disputes. It would also provide $50 million in grants for states seeking to develop or maintain an all-payer claims database.
STOP Surprise Medical Bills Act
Bipartisan legislation on surprise billing (S. 1531) was also introduced in the Senate. The STOP Surprise Medical Bills Act comes after almost a year of work from a bipartisan group of senators led by Sens. Bill Cassidy (R-La.) and Maggie Hassan (D-N.H.). While the legislation is similar to the House proposal, the bills differ in the approach taken to payment disputes.
Under the Senate bill, providers would be paid the difference between a patient’s in-network cost sharing amount and the median in-network rate for the service, but both providers and insurers would have the opportunity to appeal the payment amount through an independent dispute resolution process in which an arbiter, certified by the secretaries of Health and Human Services and the Department of Labor, must choose between the two offers. The final arbitration decision would be based upon commercially-reasonable rates for the geographic area. Patients would only owe their in network rate for the services in question, in line with the House legislation. States that have already established an alternative mechanism to address surprise insurance gaps and determine payment amounts would be able to continue with those systems under certain circumstances.
Lower Health Care Costs Act
Under the legislation (S1895), patients would be required to pay only their in-network cost-sharing amount for out-of-network emergency care and treatments provided by ancillary out-of-network providers. The proposal outlines three options for resolving payment disputes between providers and insurers: an in-network guarantee under which providers can join a health plan’s network or bill through the facility where they practice; use of an independent dispute resolution process; or payment based on the median contracted rate for the services rendered. States would have the option of enacting or continuing with current state laws or regulations. If a patient is stabilized after entering a facility through the emergency department, the patient must be given advance notice of any out-of-network care, an estimate of the cost, and referrals for alternative options for in-network care. Health plans and providers would also be required to provide patients with estimates of their out-of-pocket costs for a service within 48 hours of a request, and to send any medical bills within 30 days of the service. Insurers would be mandated to keep their provider directories up to date.
Protecting People from Surprise Medical Bills Act
The Protecting People from Surprise Medical Bills Act was introduced by Representatives Raul Ruiz, M.D., (D-CA) and Phil Roe, M.D. (R-TN) follows along the previously introduced bills with regards to removing the patient from the billing dispute. The Act takes an approach to protecting patients from surprise bills by adopting an arbitration model. Under this model – similar to the one adopted by New York State in 2015 – if providers and insurers cannot agree on a payment rate, they can engage in an independent dispute resolution process (IDR). Under IDR, insurers and out-of-network providers each identify a cost for the patient’s care, and a neutral arbiter chooses the fairer price. This model creates an incentive for both parties to choose reasonable numbers to cover the cost of treatment.
Payment Method Primer
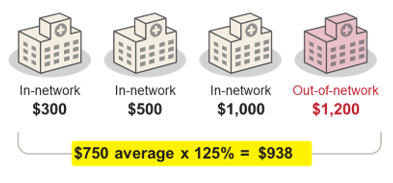
Average allowed amount
When a patient receives care from an out-of-network provider, the insurer will only pay the provider their maximum “allowed amount” for the service, which is often less than the provider is charging.
One method of determining a reasonable price for the service is to calculate the average allowed amount that the insurer pays providers in a given geographic area, including their contractually set rates with in-network providers.